Fecal Microbiota Transplantation in Treating Immune Deficiency Disorders
Fecal Microbiota Transplantation represents a promising frontier in the treatment of immune deficiency disorders, offering a novel approach to restoring immune function by modulating the gut microbiome. .
Dr Kenan Yüce
8/25/20243 min read
Introduction
Immune deficiency disorders encompass a wide range of conditions characterized by impaired immune system function, which makes individuals susceptible to infections and other health complications. Traditionally, treatments for immune deficiency disorders have focused on managing symptoms and preventing infections, but recent research has highlighted the potential role of the gut microbiome in modulating immune responses. Fecal Microbiota Transplantation (FMT) has emerged as a novel therapeutic approach that aims to restore healthy gut microbiota, thereby potentially improving immune function in patients with immune deficiency disorders. This blog post reviews the current literature on FMT's application in immune deficiency disorders, exploring its mechanisms, benefits, and the challenges associated with this innovative treatment.
The Gut Microbiome and Immune Function
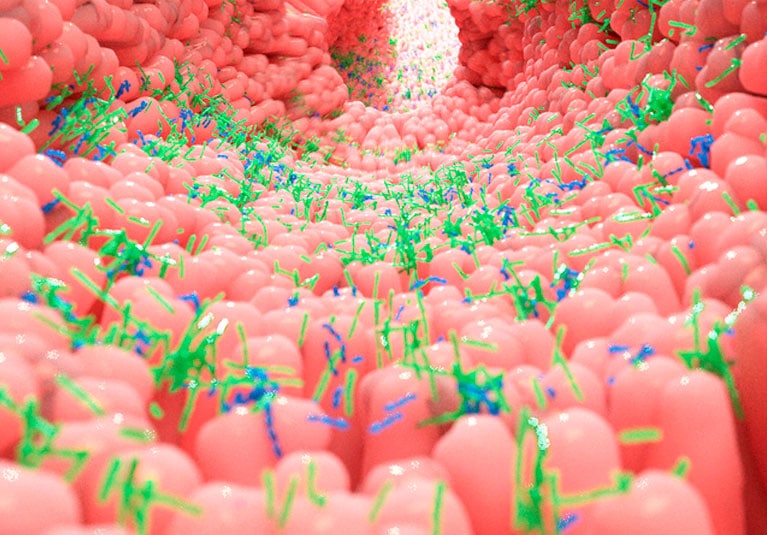
The human gut microbiome is a complex ecosystem of trillions of microorganisms, including bacteria, viruses, fungi, and archaea, which play a crucial role in maintaining overall health. Recent studies have established that the gut microbiome is intricately linked to the immune system, influencing both innate and adaptive immune responses. The gut microbiota helps in the development and maturation of immune cells, the production of antimicrobial peptides, and the regulation of inflammation.
In immune deficiency disorders, the composition of the gut microbiome is often dysregulated, characterized by a reduction in microbial diversity and an imbalance between beneficial and pathogenic bacteria. This dysbiosis can exacerbate immune dysfunction, leading to a vicious cycle where the weakened immune system further impairs microbiome health, thereby worsening the patient's condition.
Fecal Microbiota Transplantation: Mechanism of Action
FMT involves the transfer of fecal matter from a healthy donor to the gastrointestinal tract of a recipient, with the aim of restoring a balanced and diverse gut microbiota. The procedure can be performed via several routes, including colonoscopy, endoscopy, or oral capsules.
The primary mechanism by which FMT benefits patients with immune deficiency disorders is through the restoration of microbial diversity. By reintroducing a healthy and balanced microbial community, FMT can help reestablish the symbiotic relationship between the gut microbiota and the host's immune system. This, in turn, can enhance the production of essential metabolites like short-chain fatty acids, which are critical for maintaining gut barrier integrity and modulating immune responses. Moreover, FMT can reduce inflammation by suppressing the growth of pathogenic bacteria and promoting the colonization of beneficial microbes that produce anti-inflammatory molecules.
Clinical Evidence of FMT in Immune Deficiency Disorders
1. Primary Immunodeficiency Disorders (PIDs):
Research on the use of FMT in primary immunodeficiency disorders (PIDs) is still in its early stages, but there is growing interest in its potential therapeutic benefits. PIDs are a group of disorders caused by genetic defects that impair the immune system. Patients with PIDs often suffer from recurrent infections and dysbiosis. Case studies and small clinical trials have shown that FMT can help reduce infection rates and improve immune function in some patients with PIDs. For example, a study published in Frontiers in Immunology reported that FMT successfully reduced the frequency of infections in a patient with common variable immunodeficiency (CVID), a type of PID, by restoring a healthier gut microbiome.
2. Acquired Immune Deficiency Syndromes (AIDS):
HIV/AIDS is an acquired immune deficiency syndrome characterized by the progressive deterioration of the immune system. Dysbiosis is a common feature in HIV-infected individuals, contributing to chronic inflammation and disease progression. Several studies have investigated the role of FMT in HIV-positive patients, with some promising results. A study published in The Journal of Infectious Diseases demonstrated that FMT improved gut microbiota diversity and reduced markers of inflammation in HIV-infected individuals, suggesting that FMT could be a valuable adjunct therapy in managing HIV/AIDS.
3. Immune-Mediated Inflammatory Diseases (IMIDs):
Immune-mediated inflammatory diseases, such as inflammatory bowel disease (IBD), psoriasis, and rheumatoid arthritis, are often associated with immune dysfunction and gut microbiota alterations. FMT has been extensively studied in IBD, particularly in ulcerative colitis and Crohn's disease, with numerous trials demonstrating its efficacy in inducing and maintaining remission. Given the shared pathophysiological features between IBD and other IMIDs, there is potential for FMT to be explored as a treatment option for other immune-mediated disorders.
Challenges and Future Directions
Despite the promising results, several challenges remain in the application of FMT for immune deficiency disorders. One of the primary concerns is the variability in treatment outcomes, which may be influenced by factors such as donor selection, preparation methods, and the underlying condition of the patient. Standardizing FMT protocols and identifying optimal donor characteristics are essential steps toward improving the consistency and safety of this therapy.
Moreover, the long-term effects of FMT are still not fully understood, and there is a need for larger, controlled clinical trials to establish the efficacy and safety of FMT in various immune deficiency disorders. Future research should also explore the potential for personalized microbiome-based therapies, where treatments are tailored to the specific microbial and immunological profiles of individual patients.
Conclusion
Fecal Microbiota Transplantation represents a promising frontier in the treatment of immune deficiency disorders, offering a novel approach to restoring immune function by modulating the gut microbiome. While current evidence suggests that FMT can be beneficial in certain immune deficiency conditions, further research is needed to refine this therapy and fully understand its potential. For clinicians and patients considering FMT, it is crucial to weigh the potential benefits against the risks and to approach this treatment within the context of a comprehensive care plan.
