Fecal Microbiota Transplantation for Alcoholic Hepatitis
A New Hope for Patients Fecal Microbiota Transplantation offers a promising and innovative approach to treating alcoholic hepatitis. With its high safety profile, minimal risks, and substantial benefits, FMT stands out as a treatment worth considering. As research continues to evolve, FMT could become a standard therapy for alcoholic hepatitis, providing hope and improved quality of life for many patients.
Dr Kenan Yüce
7/29/20245 min read
Understanding Alcoholic Hepatitis
What is Alcoholic Hepatitis?
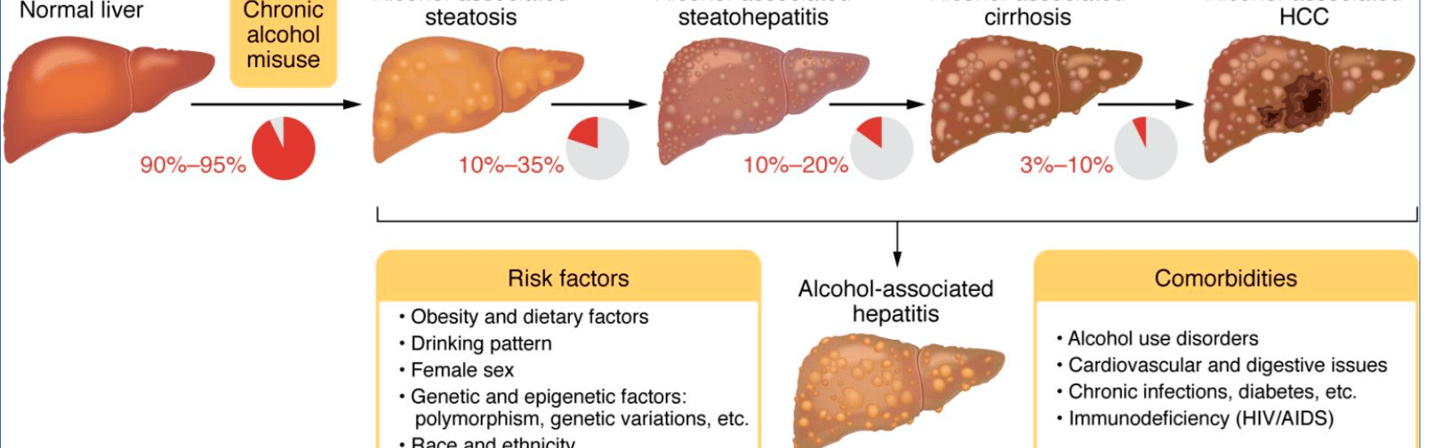
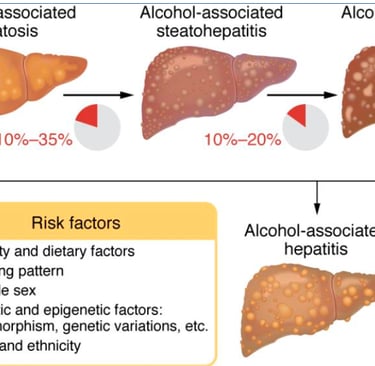
Alcoholic hepatitis is a severe inflammatory condition of the liver caused by excessive alcohol consumption. It ranges from mild to severe and can progress to cirrhosis, liver failure, and even death if left untreated. Symptoms often include jaundice, fever, abdominal pain, and liver dysfunction. Despite its severity, the standard treatments are limited and often not very effective, highlighting the need for innovative therapies.
Why Choose Fecal Microbiota Transplantation?
Fecal Microbiota Transplantation (FMT) involves the transfer of stool from a healthy donor into the gastrointestinal tract of a patient. This procedure aims to restore the balance of gut microbiota, which is crucial for maintaining various bodily functions, including immune responses and metabolic processes. The liver, as the first line of filtration between the gut and the rest of the body, is most exposed to changes in the gut microbiome and therefore more susceptible to dysbiosis.The gut microbiome plays a significant role in liver health, and its imbalance is often linked to liver diseases, including alcoholic hepatitis.
The Science Behind FMT
The current standard of care for severe alcoholic hepatitis has several limitations, such as only one-third of patients being eligible for steroid therapy. Additionally, steroids have their own issues: some patients are unresponsive, those who do respond have questionable long-term benefits, and a significant portion are not suitable for steroid treatment at all, leaving them with limited definitive treatment options. Therefore, there is a considerable gap between the problem and existing solutions. Alcohol induces dysbiosis and disrupts gut barrier function, thereby promoting the transport of microbial lipopolysaccharides to the portal circulation and liver. Hence, probiotics, prebiotics, antibiotics or fecal microbiota transplantation (FMT) may alleviate dysbiosis-related liver damage. FMT is expected to play a role in managing alcoholic liver disease overall and particularly severe alcoholic hepatitis by correcting the primary dysbiosis.Studies have shown that patients with alcoholic hepatitis often have a disrupted gut microbiome, which contributes to inflammation and liver damage. FMT can help re-establish a healthy microbiome, reducing inflammation and promoting liver regeneration. By introducing beneficial bacteria, FMT can modulate the immune response and improve liver function.
The Benefits of FMT in Alcoholic Hepatitis
Safety and Efficacy
FMT is generally considered a safe procedure with minimal side effects. It has been successfully used to treat Clostridium difficile infections, and recent studies suggest it could be beneficial for other conditions, including alcoholic hepatitis. The risk of serious adverse events is low, making it an attractive option for patients with limited treatment choices. The most common form of alcoholic liver disease, alcoholic hepatitis, has a very high short-term mortality rate of up to 50% and there is no specific treatment available other than steroids. Steroids also show limited benefit in improving short-term survival and there is no evidence of any long-term benefit. In addition, only a small proportion of patients with alcoholic hepatitis are suitable for steroid therapy. Therefore, a large number of patients are either unsuitable or unresponsive to steroids, and this group is larger than those who respond to steroids, leaving us with no specific treatment options for the majority of these individuals [2]. In most cases, liver transplantation may not even be feasible due to the presence of sepsis or recent alcohol consumption and despite documented safety and survival benefits from early liver transplantation in patients with severe alcoholic hepatitis (SAH) who do not respond to medical therapy [3], there are many ethical and logistical issues involved. Therefore, there is a need for newer, more effective non-transplant therapeutic options to manage severe alcoholic hepatitis. Intestinal dysbiosis, leaky gut, and the products of the intestinal microbiome reaching the liver are major culprits in the development of alcoholic hepatitis [4], so targeting qualitative and quantitative changes in the gut microbiome continues to be an important strategy in developing new treatments for alcoholic hepatitis [5]. Among others, modulation of the gut microbiota through fecal microbiota transplantation (FMT) has recently been conceptualized and evaluated as a potential treatment strategy in both preclinical and clinical studies.
Clinical Evidence
Several studies have explored the potential of FMT in treating alcoholic hepatitis. A notable study published in the journal Hepatology demonstrated that FMT significantly improved liver function and reduced inflammation in patients with severe alcoholic hepatitis. Another study found that FMT led to a higher survival rate compared to standard treatments. These findings underscore the potential of FMT as a viable treatment option.
Expected Success and Results
Promising Outcomes
Patients undergoing FMT for alcoholic hepatitis have shown remarkable improvements in liver function tests, reduced levels of inflammatory markers, and better overall health outcomes. The procedure can lead to rapid and sustained recovery, providing a new lease on life for those suffering from this debilitating condition. This procedure may lead to rapid and sustained improvement, offering new hope for those suffering from this debilitating condition. In a small study of 61 patients with biopsy-confirmed severe alcoholic hepatitis, Dr. C A Philips reported that patients treated with FMT experienced significantly fewer hepatic encephalopathy, critical infections, hospitalizations, and alcohol relapses compared to those treated with corticosteroids or standard care.
Long-term Benefits
The benefits of FMT extend beyond immediate recovery. By restoring a healthy gut microbiome, FMT can potentially prevent the recurrence of alcoholic hepatitis and other related liver diseases. This long-term impact makes FMT a valuable addition to the therapeutic arsenal for liver conditions.
Conclusion
A New Hope for Patients
Fecal Microbiota Transplantation offers a promising and innovative approach to treating alcoholic hepatitis. With its high safety profile, minimal risks, and substantial benefits, FMT stands out as a treatment worth considering. As research continues to evolve, FMT could become a standard therapy for alcoholic hepatitis, providing hope and improved quality of life for many patients.
Consider FMT
If you or a loved one is struggling with alcoholic hepatitis, consider discussing FMT with your healthcare provider. This cutting-edge treatment could be the key to better health and recovery. Stay informed, explore your options, and take a proactive step towards managing your condition with the latest medical advancements.
References:
1. Fecal microbiota transplantation in alcohol related liver diseases, S. M. Sasthry, Clin Mol Hepatol. 2020 Jul;26(3):294-301. PMC7364360
2. How faecal transplants can save the liver in patients of alcoholic hepatitis, The Indian express Anonna Dutt J.of Courage, New Delhi, March 12, 2023
3. FMT Benefits Last a Few Years in Severe Alcoholic Hepatitis Patients, Molly Walker, MedPage TodayNovember 14, 2021
4. Fecal Microbiota Transplantation Compared with prednisolone in Severe Alcoholic Hepatitis patients: A Randomized Trial, A.Pande, Hepatol Int. 2023 Feb;17(1):249-261.
5. Long-term Outcomes of Stool Transplant in Alcohol-associated Hepatitis—Analysis of Clinical Outcomes, Relapse, Gut Microbiota and Comparisons with Standard Care. Original Article. A.Philips, Journal of Clinical and Experimental Hepatology, Volume 12, Issue 4, July–August 2022, Pages 1124-1132
6. Long-term Outcomes of Fecal Microbiota Transplantation in Patients With Cirrhosis, Gastroenterology. Volume 156, Issue 6, May 2019, Pages 1921-1923.e3
7. Fecal Microbiota Transplantation in Liver Cirrhosis.A.Boicean, Biomedicines 2023, 11(11), 2930; https://doi.org/10.3390/biomedicines11112930
